23 Jul Telemedicine, Wearables &mHealth: Transforming Healthcare Access for the Vulnerable Populations
By 2030, nearly 2.5 billion people could be left behind by the global healthcare system due to geographic, economic, and digital divides. Today, vulnerable populations including the rural poor, elderly, refugees, and underserved urban communities, ace disproportionate barriers to healthcare access.
According to the World Health Organization (2024), over 400 million people globally still lack access to essential health services, while 45% of low-income populations remain without consistent care access.
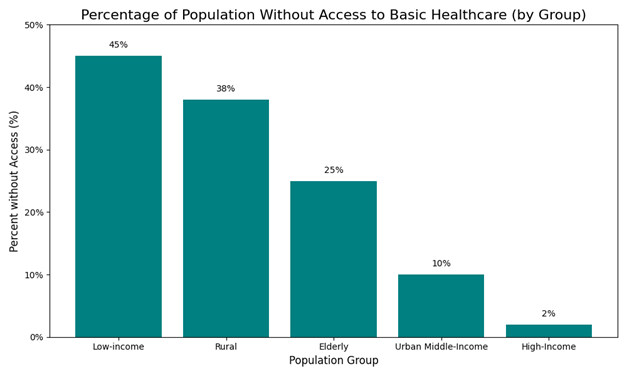
Source: World Health Organization, OECD, World bank
*Population groups are defined as follows: “Low-income” refers to individuals living below the international poverty line (approx. $2.15/day, World Bank); “Rural” includes residents in remote or non-urban areas with limited health infrastructure (WHO definition); “Elderly” includes persons aged 65 and above with age-related access challenges; “Urban middle-income” represents residents of cities with household incomes between the 40th–80th national percentiles; and “High-income” includes individuals in the top 20% income bracket with greater access to private or premium healthcare services.
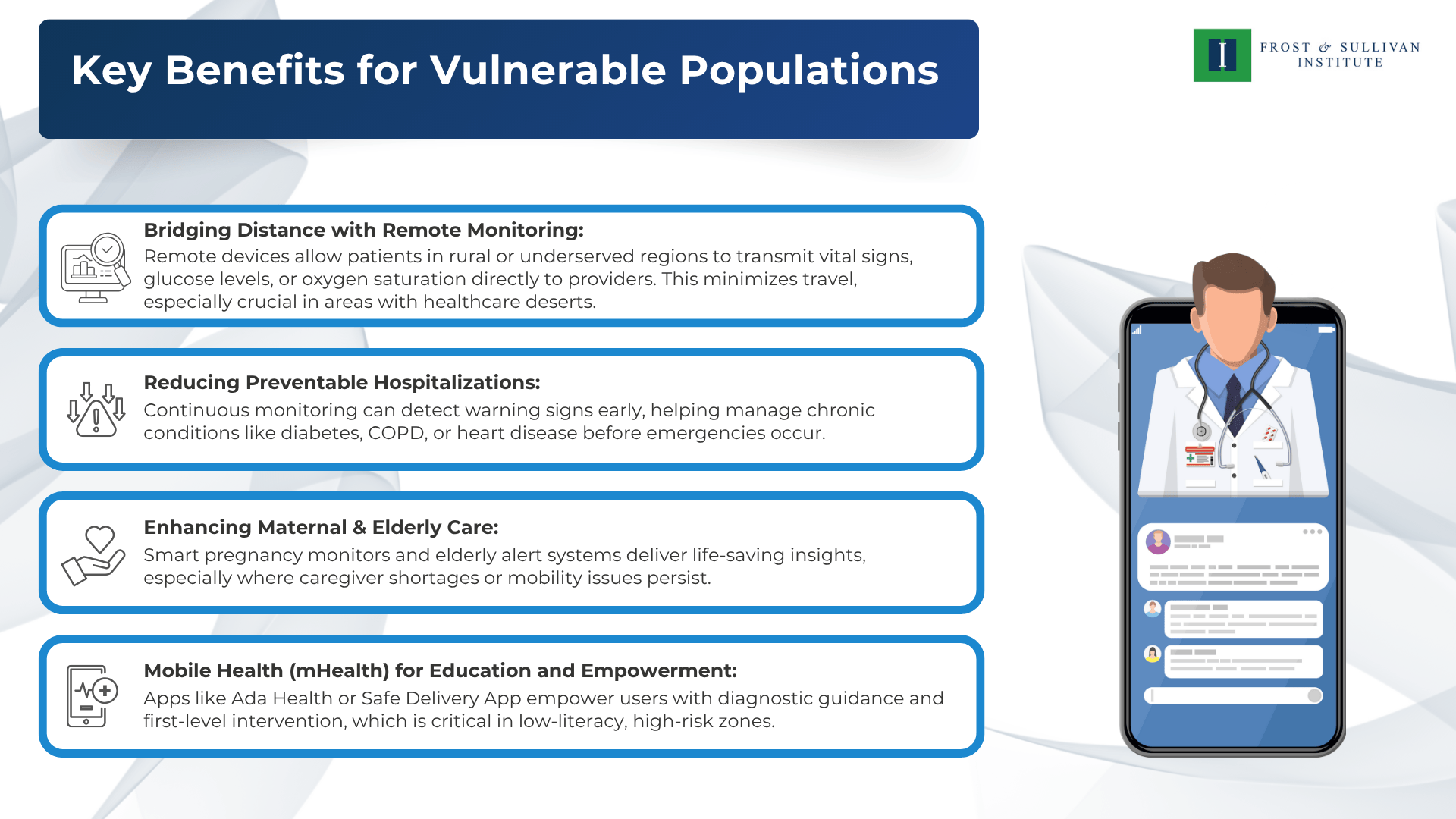
These disparities result in late diagnoses, increased mortality, and long-term socioeconomic burdens. However, connected health devices, ranging from wearables to remote diagnostics are emerging as vital tools in reversing this trend.
Connected Devices: Revolutionizing Access to Healthcare
Connected devices are internet-enabled technologies that collect and transmit health data in real-time. Their use surged after the COVID-19 pandemic, and today, over 60% of healthcare providers globally incorporate at least one form of connected care into their practice.
From mobile health apps to wearable ECGs, these tools bridge care gaps for vulnerable groups and redefine the traditional care model.
Market Trends and Adoption
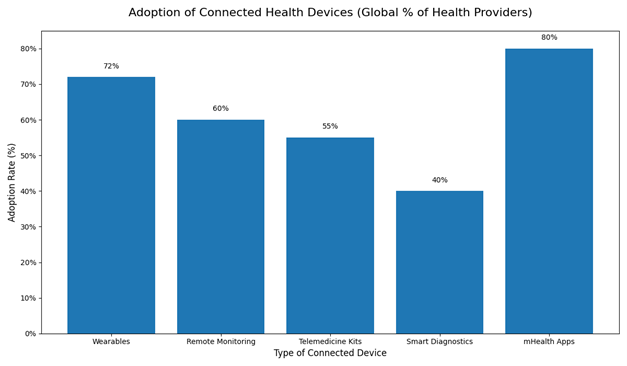
Source: Statista, Fortune Business Insights, GSMA, WHO
*Wearables track health metrics via fitness bands or smartwatches; Remote Monitoring devices capture vitals like blood pressure or glucose from home; Telemedicine Kits enable virtual exams using home-based diagnostic tools; Smart Diagnostics include connected lab tools and drones that transport test samples, kits, or medicines for faster diagnosis; mHealth Apps offer health education, virtual consults, and care tracking via mobile devices.
As of 2024:
- The global remote patient monitoring market is projected to exceed $175 billion by 2027, up from $53 billion in 2022
- Telemedicine adoption surged by 38% in low- and middle-income countries post-pandemic
Mobile health apps are used by over 80% of healthcare providers, with high penetration in maternal and chronic care programs.
Significance of Technology and Impact in Telehealth Programs
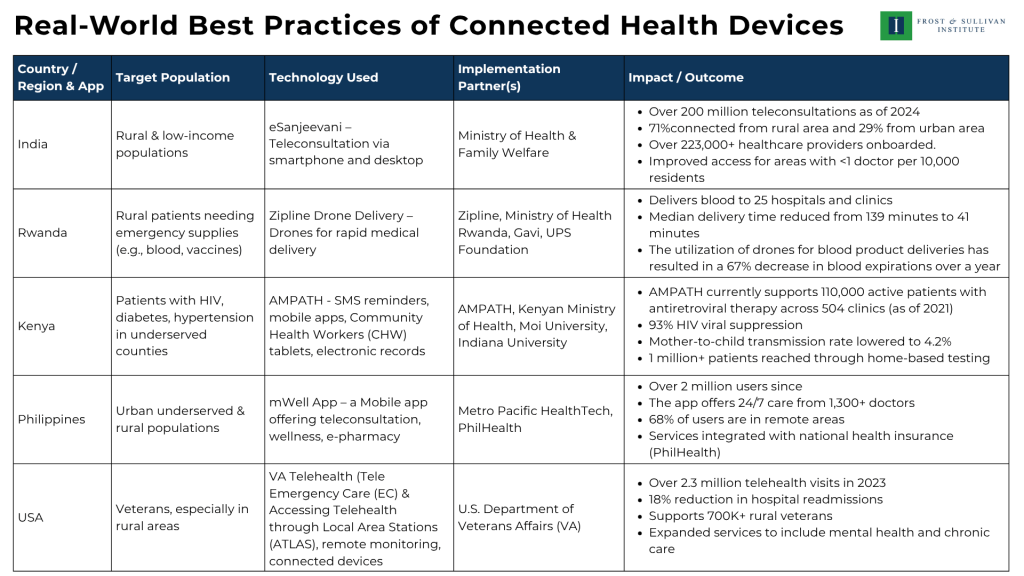
India – eSanjeevani
The eSanjeevani platform, leveraging teleconsultation via smartphones and desktops, has revolutionized healthcare access for rural and low-income populations in India. By connecting patients with over 223,000 healthcare providers, it has facilitated over 200 million teleconsultations by 2024, with 71% of users from rural areas. This technology addresses critical shortages in medical personnel, particularly in regions with fewer than one doctor per 10,000 residents, enhancing equitable healthcare delivery and reducing the need for costly travel.
Rwanda – Zipline Drone Delivery
Zipline’s drone delivery system in Rwanda employs cutting-edge drone technology to deliver emergency medical supplies, such as blood and vaccines, to rural patients. By reducing median delivery times from 139 minutes to 41 minutes, it ensures timely access to life-saving resources across 25 hospitals and clinics. The 67% reduction in blood expirations highlights the system’s efficiency, optimizing resource use and improving health outcomes in remote areas with limited infrastructure.
Kenya – AMPATH
AMPATH in Kenya integrates SMS reminders, mobile apps, Community Health Worker tablets, and electronic records to manage chronic conditions like HIV, diabetes, and hypertension in underserved counties. Supporting 110,000 patients across 504 clinics with a 93% HIV viral suppression rate and reducing mother-to-child transmission to 4.2%, this technology-driven approach enhances patient adherence and care coordination. Reaching over 1 million through home-based testing, it significantly expands healthcare access in resource-constrained settings.
Philippines – mWell App
The mWell app in the Philippines uses mobile technology to provide teleconsultation, wellness services, and e-pharmacy to urban underserved and rural populations. With over 2 million users, 68% from remote areas, and 24/7 access to 1,300+ doctors, it bridges geographical gaps in healthcare. Integration with PhilHealth ensures affordability, amplifying its impact by making comprehensive care accessible to populations previously underserved by traditional healthcare systems.
USA – VA Telehealth
The U.S. Department of Veterans Affairs’ Telehealth program, including Tele Emergency Care and ATLAS, utilizes telehealth portals, remote monitoring, and connected devices to serve over 700,000 rural veterans. With 2.3 million telehealth visits in 2023 and an 18% reduction in hospital readmissions, this technology enhances chronic care and mental health services. By overcoming geographical barriers, it ensures timely, high-quality care for veterans, improving health outcomes and system efficiency.
Connected Devices as a Critical Enabler of Equitable Healthcare
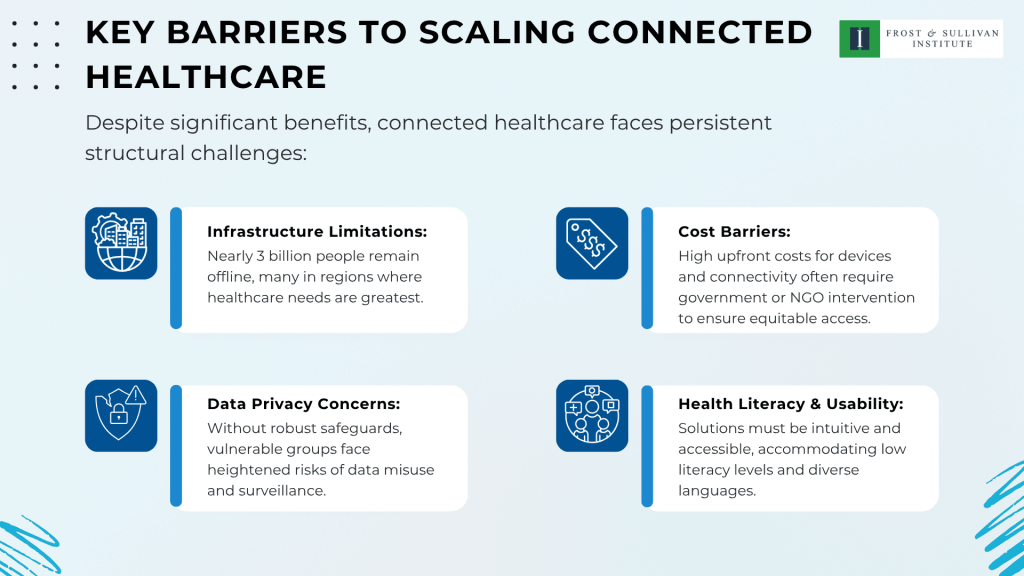
The integration of connected health technologies is no longer a futuristic concept; it is a necessary step toward equitable healthcare delivery. For vulnerable populations, these innovations are helping bridge long-standing gaps caused by geography, poverty, and limited infrastructure. From enabling remote diagnostics in rural India to improving medication adherence in underserved communities in Kenya, the real-world impact is both measurable and meaningful.
However, the full potential of connected devices can only be realized through multi-stakeholder commitment. Expanding digital infrastructure, ensuring affordability, upholding data privacy, and designing for inclusivity are critical to scale these solutions responsibly.
As we move closer to 2030, connected devices will play an increasingly central role in reaching those most at risk of being left behind. Accelerating their adoption ethically, inclusively, and sustainably offers a powerful path to advancing universal health coverage and strengthening health systems globally.
Blog by Asha Sridar,
Manager, Frost & Sullivan Institute