27 Jun Ultraportable Medical Imaging: Expanding Healthcare Access in Remote and Underserved Areas
The Global Health Equity Crisis
Despite decades of global health interventions, more than half of the world’s population still lacks access to essential healthcare services, according to the World Health Organization (WHO). Rural and remote regions continue to face significant disparities in healthcare access, with 56% of rural residents lacking essential healthcare services. Despite overall progress, primary healthcare (PHC) inequalities remain particularly severe in remote rural areas, where geographic isolation and limited infrastructure hinder service delivery. A study from rural China found that healthcare centers equipped with more advanced medical equipment are associated with improvements in the overall infrastructure of village clinics, highlighting the critical role of diagnostic and treatment technology in strengthening rural healthcare systems.
In lower- and middle-income countries (LMICs), access to medical imaging remains severely limited
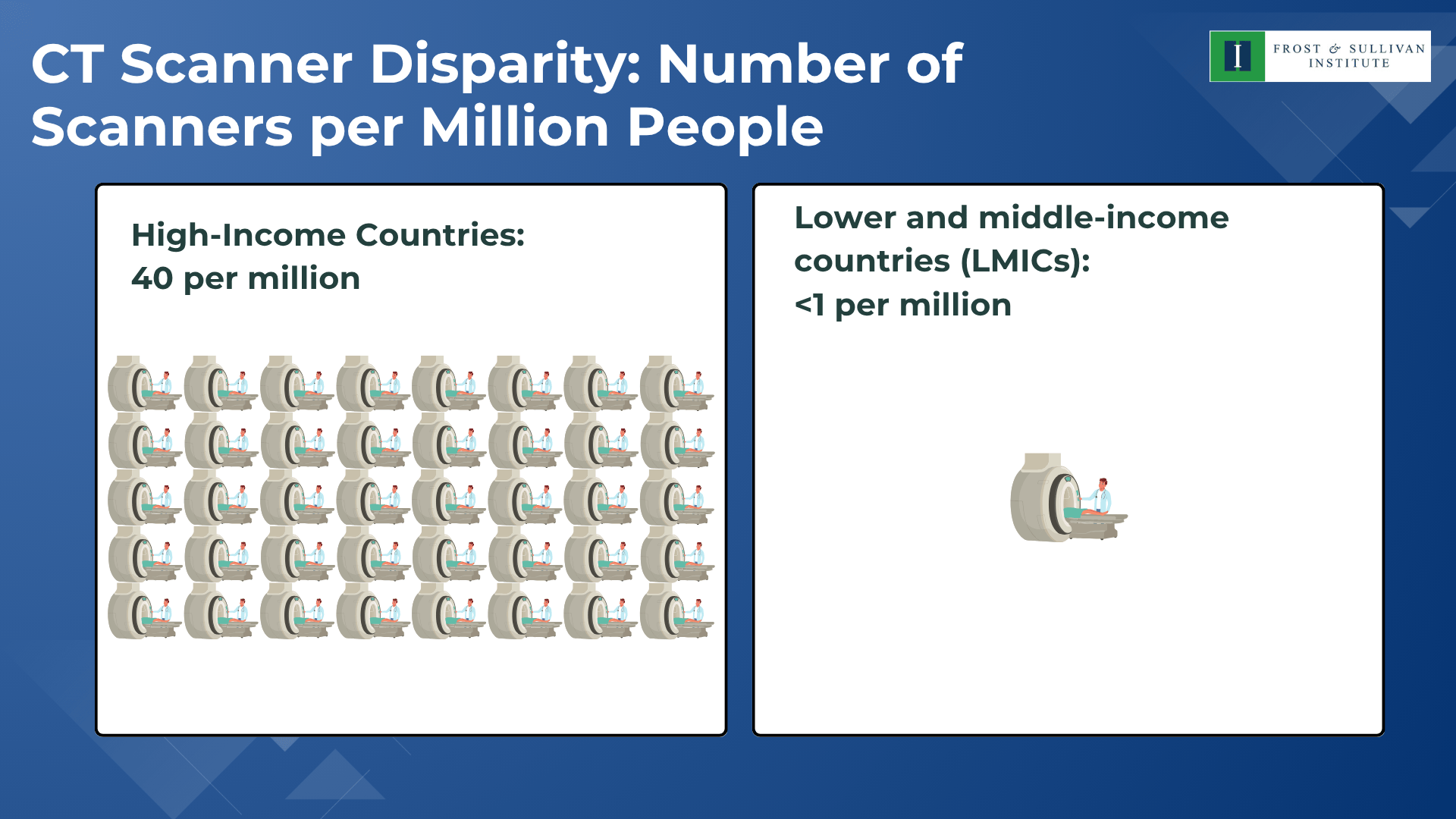
The disparities are even wider for MRI and other specialized diagnostic equipment. This lack of imaging infrastructure delays or prevents timely diagnoses, worsening patient outcomes and placing additional long-term strain on already overburdened healthcare systems. The growing burden of non-communicable diseases and aging populations in these regions only exacerbates the need for scalable diagnostic solutions.
This crisis calls for radical innovation in decentralized, accessible, and mobile diagnostic solutions.
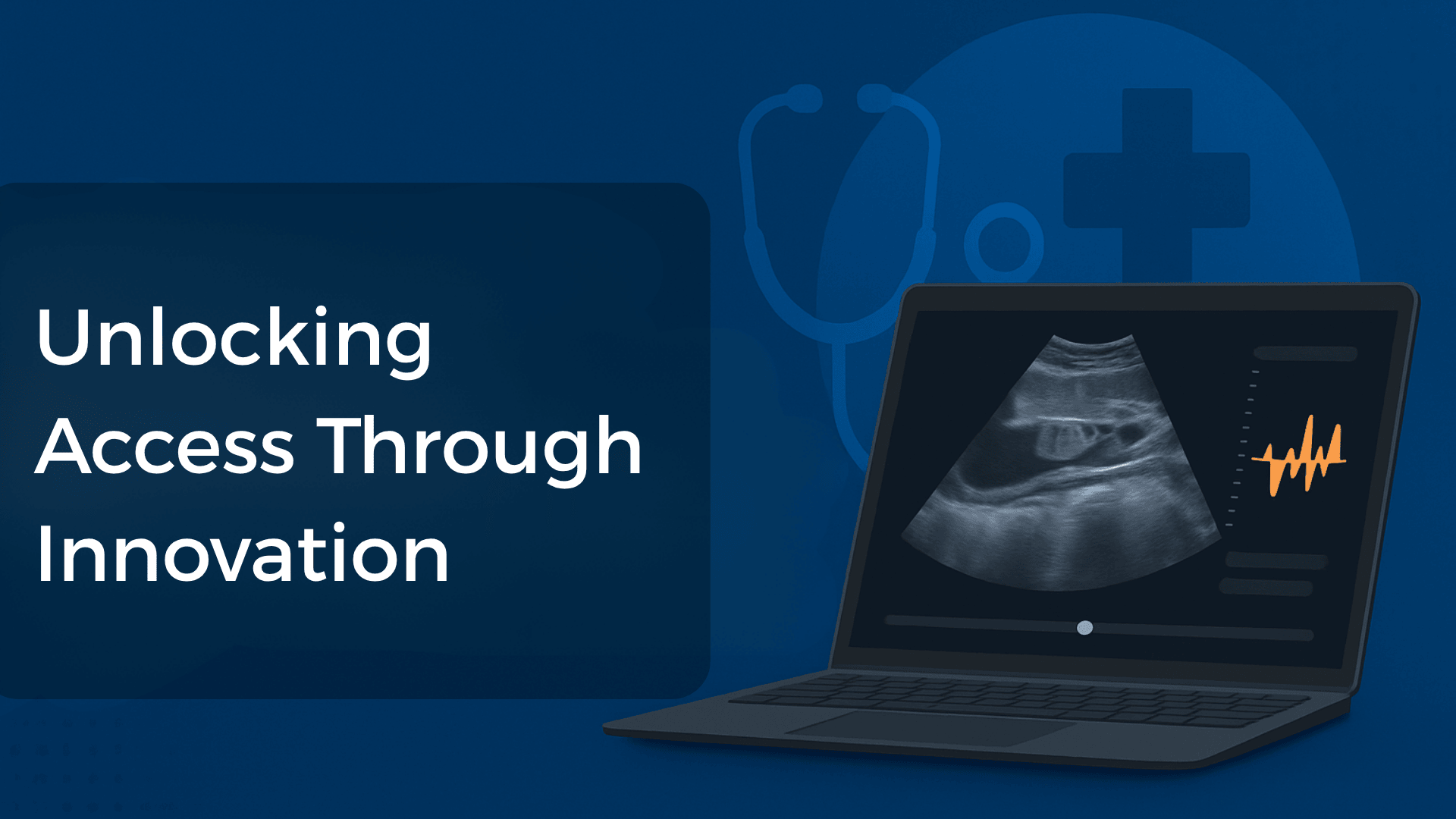
When Distance Meets Diagnosis: The Rise of Ultraportable Medical Imaging
Ultraportable Medical Imaging (UMI) devices—such as handheld ultrasounds, mobile X-ray units, and battery-powered MRIs—represent a revolution in diagnostic care delivery, especially in resource-scarce settings. By shrinking size, cost, and energy demands, UMI enables frontline health workers, mobile clinics, and telemedicine platforms to bring diagnostics directly to patients, rather than requiring patients to travel great distances.
Benefits of UMI
- Portability & Scalability: Lightweight devices (some as small as smartphones) can be carried in backpacks and deployed in ambulances, rural clinics, or disaster zones.
- Cost-effectiveness: Devices like Butterfly iQ+ are significantly cheaper than traditional machines, reducing capital investment for rural facilities.
- Real-time Diagnosis: Enables immediate image capture and cloud-based analysis via AI or remote radiologists.
- Energy Independence: Operates on battery or solar power—critical in regions with unreliable electricity.
- Training Simplification: Many UMI tools use AI to guide non-specialists, reducing dependency on radiologists.
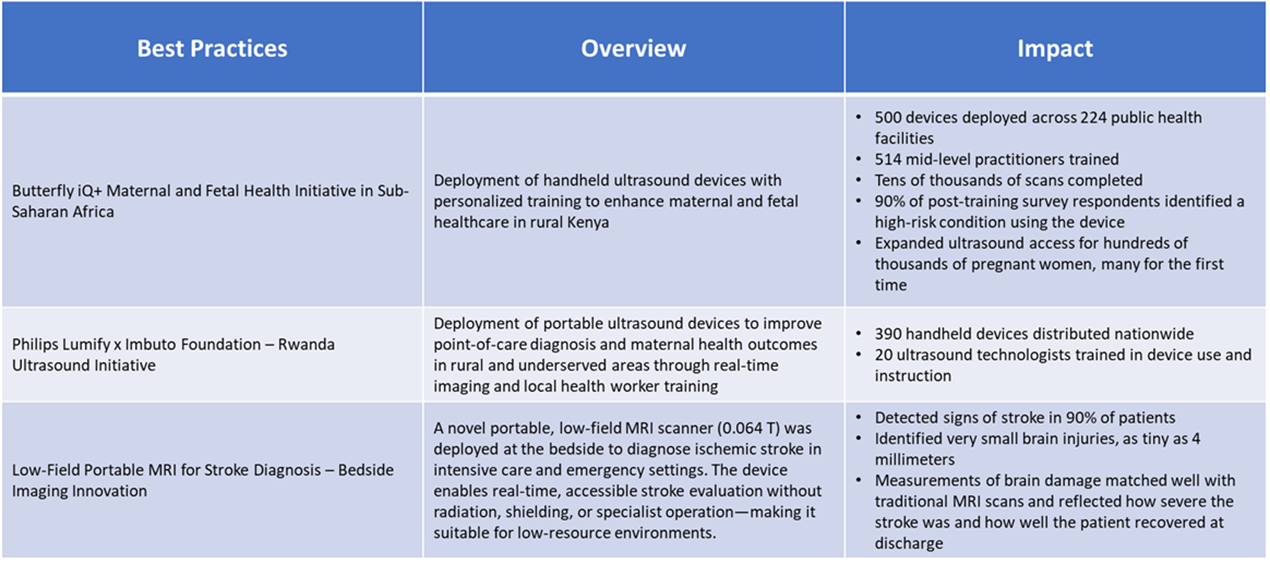
Realizing the full potential of ultraportable imaging requires more than innovation—it demands strategic integration into healthcare delivery. The following best practices outline how to ensure effectiveness, sustainability, and equity in implementation.
Barriers to Global Replication
While UMI technology is transformative, several hurdles remain:
- Infrastructure Gaps: Even portable devices require minimal connectivity or cloud storage, which is unavailable in some isolated regions.
- Training and Adoption: Despite AI assistance, correct imaging capture and interpretation still require basic skillsets that must be built locally.
- Policy and Regulation: Varying medical device approval frameworks hinder cross-border deployment.
- Data Privacy and Cloud Access: Secure transmission and storage of patient data remain a concern, especially with cloud-based diagnostics.
- Cost and Scale: While cheaper than conventional machines, UMIs still require upfront investment that might be challenging for community clinics or local governments.
A Diagnostic Revolution in Progress
Ultraportable Medical Imaging offers one of the most promising pathways to universal diagnostic coverage, particularly in hard-to-reach geographies. When paired with digital infrastructure, task-shifting, and supportive regulation, UMI can be the bridge between rural isolation and modern medicine.
At the Frost & Sullivan Institute, we believe that technologies like UMI are pivotal to achieving healthcare equity, especially in remote and rural areas. However, technology alone is not enough. A multi-stakeholder approach—combining innovation, partnerships, policy reform, and local capacity building—is essential for real-world impact.
The future of diagnostics no longer lives in distant labs—it now fits in our hands. The real journey begins when it reaches those furthest from care.
Blog by Sakthi Kumararaja,
Associate, Frost & Sullivan Institute